Overactive Bladder
Overview
What is Overactive Bladder
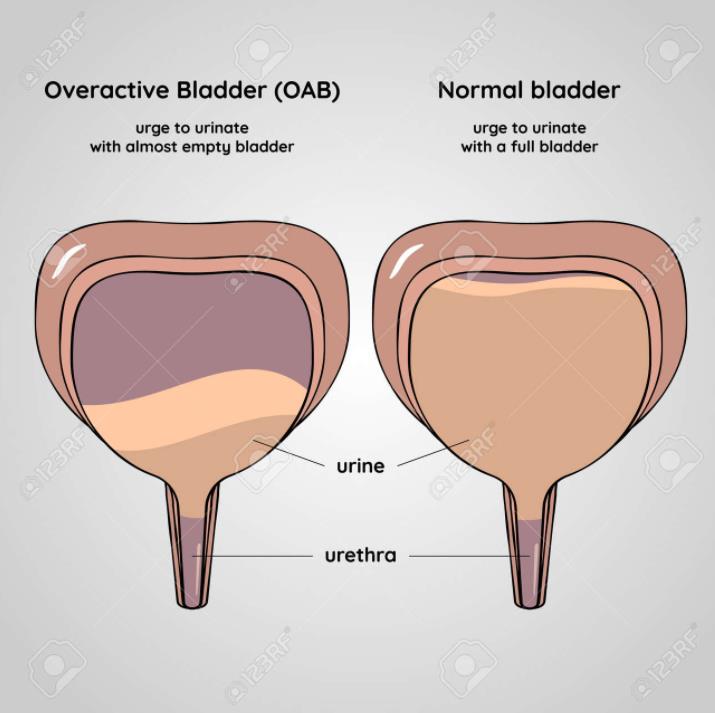
An overactive bladder is when the bladder contracts suddenly without your control, and when the bladder is not full. Often known as overactive bladder syndrome, it is a common condition where no cause can be found for the repeated and uncontrolled bladder contractions. (It is not due to a urine infection or an enlarged prostate.)
Symptoms
Whilst symptoms vary from person to person, they tend to occur in approximately one in six people. Symptoms may include:
- Frequency – going to the toilet more than seven times a day and in many cases a lot more than seven times a day.
- Urgency – getting a sudden urgent desire to pass urine, not being able to put off going to the toilet.
- Nocturia – waking to go to the toilet more than once at night.
- Urge incontinence – occurs in some cases. Urine can leak before you can get to the toilet when you have a feeling of urgency.
Causes
The bladder muscle seems to become overactive and contract (squeeze) when it should not, but the cause is not fully understood.
Normally, the bladder muscle (detrusor) is relaxed as the bladder gradually fills up. As the bladder gradually stretches, you get a feeling of wanting to pass urine when the bladder is about half full.
Most people can hold easily for some time after this initial feeling until it is convenient to go to the toilet. In people with an overactive bladder, the bladder muscle seems to give incorrect messages to the brain. The bladder may feel fuller than it actually is. The bladder contracts when it is not very full, and not when you want it to. This can result in a sudden urge to go to the toilet. In effect, you have much less control over when your bladder contracts to pass urine.
Diagnosis
If you have an abnormal urge to urinate, your doctor will check to make sure that you don’t have an infection or blood in your urine. Your doctor may also want to make sure that you’re emptying your bladder completely when you urinate.
Your doctor will look for clues that might also indicate contributing factors. Your appointment will likely include a:
- Medical history
- Physical exam, which may include a rectal exam and a pelvic exam in women
Treatment
General lifestyle measures:
- Getting to the toilet – make this as easy as possible. If you have mobility trouble, consider special adaptations like a raised seat or handrail or in your toilet. Sometimes a commode in the bedroom can make life much easier.
- Caffeine – this has a diuretic effect, making urine form more often. Caffeine may also directly stimulate the bladder making urgency symptoms worse. It may be worth trying to go without caffeine for a week or so to see if your symptoms improve. If symptoms do improve, you may not want to give up caffeine entirely, though you may wish to limit or change the times that you have caffeine. You should also try and plan to be near to a toilet whenever you have caffeine.
- Alcohol – in some people, alcohol worsens symptoms.
- Drink normal quantities of fluids – it may seem sensible to cut back on the amount of liquid you drink so the bladder does not fill so quickly. However, this can also make symptoms worse as the urine becomes more concentrated, which may irritate the bladder muscle. Aim to drink around two litres (about 6-8 cups) of fluid per day and more in hot climates and hot weather.
