Prostate Cancer
Overview
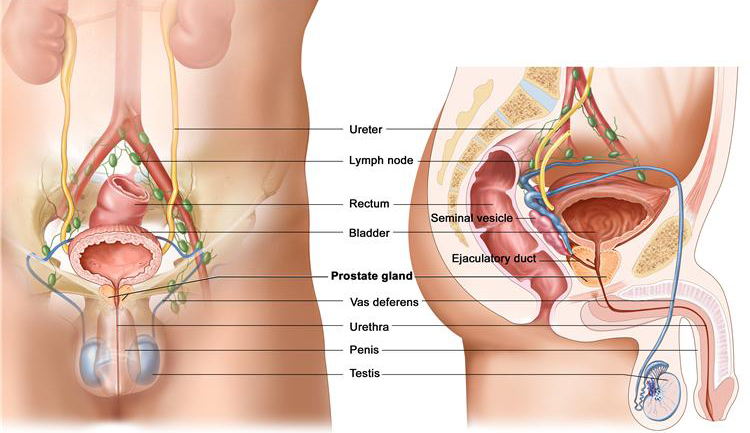
What is Prostate Cancer
Being the most common form of cancer in men, over 40,000 men are diagnosed with prostate cancer every year. An estimated 50% of men over 50 are diagnosed with prostate cancer and this figure increases to 80% in men over 80. In most cases these cancers lay dormant and will grow slowly particularly in elderly men. However in some less common cases these cancer cells are known to be megastatic (spreading) and can move to other areas of the body.
Symptoms
- Frequent urination
- Difficulty maintaining a steady stream of urine
- Having to urinate during the night
- Blood in the urine
- Change in sexual function and performance
There are many factors that will affect the risk of having cancer. Generally speaking men with a family history of prostate cancer will be 2 to 3 times more likely to get it themselves.
Causes
Prostate problems are common; 1 in 5 men will develop prostatic symptoms and 1 in 6 will develop prostate cancer, which is now the most frequent cancer in men.
It’s not clear what causes prostate cancer. Doctors know that prostate cancer begins when cells in the prostate develop changes in their DNA. A cell’s DNA contains the instructions that tell a cell what to do. The changes tell the cells to grow and divide more rapidly than normal cells do. The abnormal cells continue living, when other cells would die.
Diagnosis
There are many tests that can gather information about the prostate and urinary tracts. There are less evasive methods such as Ultrasound, CT scans and cytoscopy. There is one test that can confirm the presence of cancerous cells in the body, which is a biopsy. A doctor will remove a small piece of the prostate to examine under microscope.
In some cases, it may be possible to avoid a biopsy. The Hospital is able to offer the most modern prostate imaging using our MRI scanner. The multiparametric 3T MRI offers improved accuracy in the assessment of small areas of prostate tumour and to assess any potential spread. This enables more superior and personalised care.
Treatment
Non surgical options:
There are many non-surgical treatment options available for Peyronie’s disease but they have not proven to work for all patients. These include:
- Medication – oral and/or topical medication.
- Injections – medicine injected into the plaques, may improve pain, the size of the plaques and the amount of bend in the penis.
- Stretching – or external penile traction, which involves wearing a device which stretches the penis, with the aim of improving the length of the penis and reducing the deformity.
- Vacuum devices – these stretch the shaft by creating a vacuum around the penis.
